There are several things you can do to keep your asthma well controlled. These include learning about your condition, understanding how and when to use all your medications (and when to seek emergency help), avoiding things that make your symptoms worse, keeping track of your symptoms, and seeing your doctor regularly for monitoring.
Education — It's important to make sure that you learn and understand:
●What asthma is – Being familiar with the definition of asthma, how to recognize symptoms, and the role of medication can empower you in taking care of yourself. This can also help family members and friends understand your condition.
●When to use your medications – Asthma medicines work in different ways, so it is important to know which medication will treat asthma symptoms quickly and which ones are used to prevent symptoms from happening. Keeping an asthma "action plan" can help prepare you to treat symptoms when they happen.
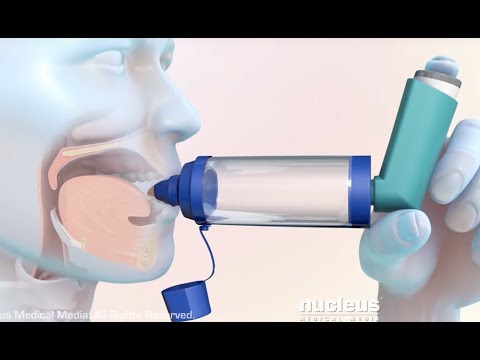
●How to use your inhalers – Many people with asthma need to use multiple inhalers, and some require different techniques. It's important to know how to use each so you get the medication you need when you need it.
●What triggers your asthma – This allows you to avoid or limit exposure to things that make your symptoms worse.
Monitoring your asthma over time — In order to successfully manage your asthma, you will need to monitor your condition over time. This involves being aware of the frequency and severity of your symptoms and measuring your lung function regularly.
Asthma diary — Your health care provider may recommend keeping a daily asthma diary when your symptoms are not well controlled or when starting a new treatment. In the diary, you can keep track of when you have symptoms (such as coughing, wheezing or shortness of breath); which medications you took and when; and your peak expiratory flow (PEF), also called "peak flow" .
Measurement of lung function — Monitoring your lung function involves measuring your PEF or forced expiratory volume in one second (FEV1), ie, the rate at which you can exhale. When asthma is causing your airways to narrow, air flows more slowly out of your lungs, causing the PEF or FEV1 measurement to be lower.
Your health care provider might suggest that you check your PEF at home periodically by blowing into a device called a peak flow meter. These devices are inexpensive and easy to use.
FEV1 is measured by spirometry. This test is usually done in a doctor’s office or pulmonary function laboratory, about every one to two years, or more often if asthma symptoms are more frequent or severe. However, it can now be done for home monitoring by patients or in conjunction with telehealth visits.
PEF and spirometry are used to monitor your lung function and response to medication, and help guide decisions regarding treatment.
Action plan — An asthma "action plan" is a form or document that your provider can help you put together; it includes instructions about how to monitor your symptoms and what to do when they happen. Different forms are available for this purpose . An action plan can tell you when to add or increase medications, when to call your provider, and when to get immediate emergency help. This can help you, or your family members, know what to do in the event of an asthma attack. Different people can have different action plans, and your action plan may change over time.
Action plans usually include three categories, based on your symptoms and/or your PEF :
●Green – Green means your lungs are functioning well. When symptoms are not present or are well controlled, you can typically continue your regular medicines and activities.
●Yellow – Yellow means your airways are somewhat narrowed, making it difficult to move air in and out; asthma symptoms may be more frequent or more severe. This is usually treated with a short-term change or increase in medication. You should change or increase your medication according to the plan that was discussed with your provider.
●Red – Red means your airways are severely narrowed and symptoms are severe; this requires immediate treatment, often with several medications.
When to call for emergency help — It's important to know when to get emergency help, for example, if your medications do not work quickly to relieve symptoms. Severe asthma attacks can lead to death if not treated promptly.
You should not attempt to drive yourself to the hospital if you are having severe asthma symptoms, and you should not ask someone else to drive. Calling for emergency help is safer than driving for two reasons:
●From the moment emergency personnel arrive, they can begin evaluating and treating your asthma. When driving in a car, treatment is generally delayed until you arrive in the emergency department.
●If a dangerous complication of asthma occurs on the way to the hospital, emergency personnel will able to treat the problem immediately. It is not safe to try to drive a car and treat a severe asthma attack at the same time.
An oral steroid medication (eg, prednisone) is often given for 5 to 10 days to treat an asthma attack and reduce the risk of a second attack.
Controlling asthma triggers — The factors that set off and worsen asthma symptoms are called "triggers." Identifying and avoiding your asthma triggers is essential in keeping symptoms under control. Common asthma triggers generally fall into several categories:
●Allergens, including dust, pollen, mold, cockroaches, mice, cats, and dogs
●Respiratory infections, such as the common cold, the flu, or COVID-19
●Irritants, such as tobacco smoke, chemicals, and strong odors or fumes
●Physical activity, especially if you are breathing cold or dry air while exercising
●Certain medications, including beta blockers (used to treat high blood pressure)
●Emotional stress
●Hormonal changes related to the menstrual cycle (in some women)
Although this is uncommon, some people develop asthma symptoms after exposure to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen.
After identifying potential asthma triggers, you and your health care provider should develop a plan to deal with the triggers.
Regular medical appointments — People with asthma need to see their health care provider regularly. For adolescents and others whose asthma is well-controlled, this may mean appointments once or twice a year. If your asthma is not well-controlled, you will likely need to go more frequently.
At these visits, your provider will ask about the severity and frequency of your asthma symptoms to assess how well your treatment is working. If your asthma has been well-controlled for at least three to six months, your provider may suggest continuing with your current treatment or possibly decreasing ("stepping down") your medication. If your provider thinks you are a candidate for stepping down, they will work with you to decide which medication(s) to decrease or stop, and monitor you closely to ensure that your symptoms remain under control.
It's important to let your provider know if your asthma symptoms get worse at any point in time. If this happens, they will review your medications, ensure that you are avoiding triggers and using your inhaler(s) properly, and suggest changes in medications or dosing as appropriate.
Sometimes other, related conditions can make asthma symptoms worse; these may need to be addressed in order to achieve good asthma control. Examples include gastroesophageal (acid) reflux (when stomach contents back up into the esophagus, causing symptoms like heartburn and regurgitation); nasal congestion or sinus disease; excess weight; and sleep apnea (a condition that makes you stop breathing for short periods during sleep).



No comments:
Post a Comment