People with persistent asthma generally need to take medication on a daily basis to keep their asthma under control, even if they do not have symptoms every day. The medications used for this are called "long-term controller" medications.
Some controller medications come in an inhaler, while others are taken as a tablet. If you take a controller medication, the type and dose will depend on how frequently you have symptoms and how severe they are. If you have severe asthma, your doctor may prescribe more than one controller medication.While controller medications help to reduce the frequency of asthma attacks, you will still need to keep quick-relief medications with you at all times, so you can treat symptoms if they do happen.
Inhaled steroids — Inhaled steroids (also known as glucocorticoids or corticosteroids) decrease inflammation (swelling) of the airways over time. The steroids used to treat asthma are entirely different from the ones athletes sometimes take to build muscle. Regular treatment with an inhaled steroid reduces the frequency of symptoms (and the need to use short-acting medication for symptom relief), improves quality of life, and decreases the risk of serious attacks.
A number of different inhaled steroid medications are available, all of which are taken once or twice a day. Sometimes, a daily steroid is prescribed along with another medication, called a long-acting bronchodilator.
Side effects — Unlike oral steroids (taken as a tablet or liquid by mouth), very little of the inhaled steroid is absorbed into the bloodstream, and there are few side effects. However, as the dose of inhaled steroid is increased, small amounts of the inhaled medication are absorbed into the bloodstream, and the risk of long-term side effects increases.
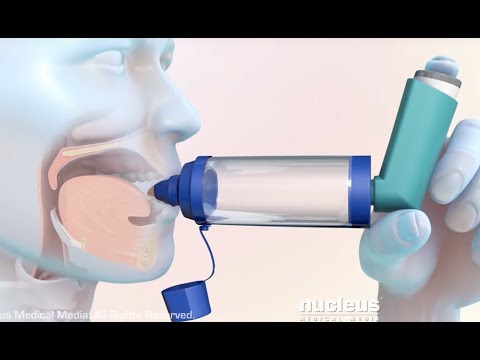
The most common side effect of low-dose inhaled steroids (as are typically used to control mild to moderate persistent asthma) is a fungal infection in the mouth called “oral candidiasis” (also known as thrush). This can usually be prevented by rinsing your mouth and gargling with water immediately after using your inhaler. If you have a metered dose inhaler, it may also help to use a spacer device; this promotes delivery of medication directly to the lungs, with less deposited in the mouth .
A hoarse voice and sore throat are less common side effects of inhaled steroids; these can often be managed by switching to a different medication or type of inhaler.
Higher doses of inhaled steroids are sometimes used to control more severe persistent asthma. Rare but possible side effects of long-term, high-dose inhaled steroid treatments, besides oral candidiasis, include cataracts, increased pressure in the eye (glaucoma), easy bruising of the skin, and increased bone loss (osteoporosis).
The risk of these complications is far less with inhaled steroids compared with oral steroids (eg, prednisone). Nevertheless, to minimize the risk, your health care provider will prescribe the lowest possible dose to control your asthma.
Inhaled steroids plus a long-acting bronchodilator — Many adults and adolescents with persistent asthma take a long-acting beta-agonist (LABA) in combination with an inhaled steroid. LABAs work for 12 or more hours, longer than short-acting beta-agonists (SABAs); they include formoterol, salmeterol, and vilanterol. An inhaler that contains both a steroid and a LABA is usually preferred (sample brand names: BUDAMATE, FORACORT, FORMOFLO, MAXIFLO, SEROFLO). An inhaler containing budesonide and formoterol (brand names: BUDAMATE, FORACORT, FOMTIDE, COMBIHALE FB) can be used as a daily controller medication and is sometimes also used for quick relief of asthma symptoms when they happen; this is because formoterol takes effect as quickly as a SABA such as Salbutamol.
Tiotropium (brand name: TIATE, TIOVA ) is another type of long-acting bronchodilator, called a long-acting muscarinic antagonist (LAMA). It is used more frequently for treating chronic obstructive pulmonary disease (COPD), but is sometimes used (along with an inhaled steroid) as an asthma controller medication if other treatments have not worked well.
Leukotriene modifiers — Leukotriene modifiers are long-term controller medications that you take as a tablet, rather than through an inhaler. They include montelukast (brand name: MONTAIR, TELEKAST, MONTEK), zafirlukast . Leukotriene modifiers work by opening narrowed
airways, decreasing inflammation, and decreasing mucus production. They may be an alternative to inhaled steroids for mild asthma, and they have few side effects (occasionally, agitation or depression can occur). However, they are less effective in controlling asthma. They are sometimes used in addition to inhaled steroids for more severe asthma.
Leukotriene modifiers can be used to prevent symptoms before exposure to a trigger or before exercising; however, they need to be taken two or more hours in advance.